America, along with the rest of the world, is working swiftly to develop a vaccine against SARS-CoV-2, the new coronavirus responsible for COVID-19.
Many people are pinning their hopes on the development of a safe and effective vaccine for COVID-19 that can stop the spread of the virus. Through its Operation Warp Speed initiative, the Trump administration is investing billions of dollars to accelerate efforts in the U.S. to develop, manufacture and distribute such vaccines.
But despite the efforts to work quickly, safety remains the top priority of researchers in the U.S.
“We are moving as quickly as we can to shorten the timelines to get a vaccine to the public, but we will not compromise one iota the multiple safety checks and safety processes that we have always had in place for vaccine development and testing,” says Kayvon Modjarrad, director for emerging infectious diseases at the U.S. Army’s Walter Reed Army Institute of Research, which is working to develop a vaccine for COVID-19. “We cannot and will not take any shortcuts when it comes to safety assessments of the vaccines we are advancing.”
“The FDA [U.S. Food and Drug Administration] will only approve or make available a COVID-19 vaccine if we determine that it meets the high standards that people have come to expect of the agency,” said Peter Marks, director of the FDA’s Center for Biologics Evaluation and Research.
How vaccines are developed
Vaccines typically take years to develop, and extensive testing is built into the process. In the U.S., promising vaccines developed in the lab move on to animal studies, followed by human studies called clinical trials. The FDA sets guidelines for the three phases of clinical trials, with each phase increasing in population size. Phase 3 clinical trials, for example, typically involve thousands of volunteers receiving the test vaccine.

Scientists and lab technicians at the Walter Reed Army Institute of Research work to counter threats of emerging infectious diseases to U.S. forces. (U.S. Army/Shawn Fury)
If the clinical trials show that the vaccine is effective without harmful side effects, the vaccine manufacturer can apply for FDA approval to publicly administer it. Even after the vaccine is in widespread use, the federal government continually monitors it for adverse effects.
History shows the potential risks associated with vaccine development. A polio vaccine developed by renowned scientist Jonas Salk was licensed for public use in 1955, but a production error caused some batches of the vaccine to contain the live virus. The incident led to increased quality-control measures in the U.S., to ensure safe immunization of children.
“People’s lives are too important for us to cut corners on the safety side of things.”
— Robert Hopkins, chair of the National Vaccine Advisory Committee
Today, the FDA’s Center for Biologics Evaluation and Research oversees vaccine safety and reviews and licenses vaccine candidates in the U.S.
David Jones, a professor of the history of science at Harvard University, says vaccine development is inherently safer than in the past. Rather than live virus, most vaccines contain either an inactivated form of the virus or a specific protein of the virus that is used to trigger the body’s immune response.
New candidate COVID-19 vaccines, including those in development by Moderna and Pfizer/BioNtech, are exploring new technologies using the virus’s genetic code.
Nevertheless, safety is critical. “There’s a tremendous amount at stake,” says Jones. If a vaccine is developed without safety at the forefront of the process, it could harm people’s health and create a loss of trust. “That could potentially decrease vaccination rates for polio, measles and everything else,” says Jones.
Speed with safety
The U.S. is working to shorten the path to a COVID-19 vaccine without compromising safety, says Robert Hopkins, chair of the National Vaccine Advisory Committee, which advises the U.S. Department of Health and Human Services’ National Vaccine Program on development and safety.
“What’s being done with Operation Warp Speed and a lot of our current vaccine trials is that we’re taking some of those [usual] steps and instead of doing them one after the other, we’re doing some of them in parallel,” says Hopkins. “We are doing things in a slightly different sequence in order to get to the end point more rapidly, but that doesn’t mean we’re cutting out any of the steps when it comes to assessing safety and efficacy. People’s lives are too important for us to cut corners on the safety side of things.”
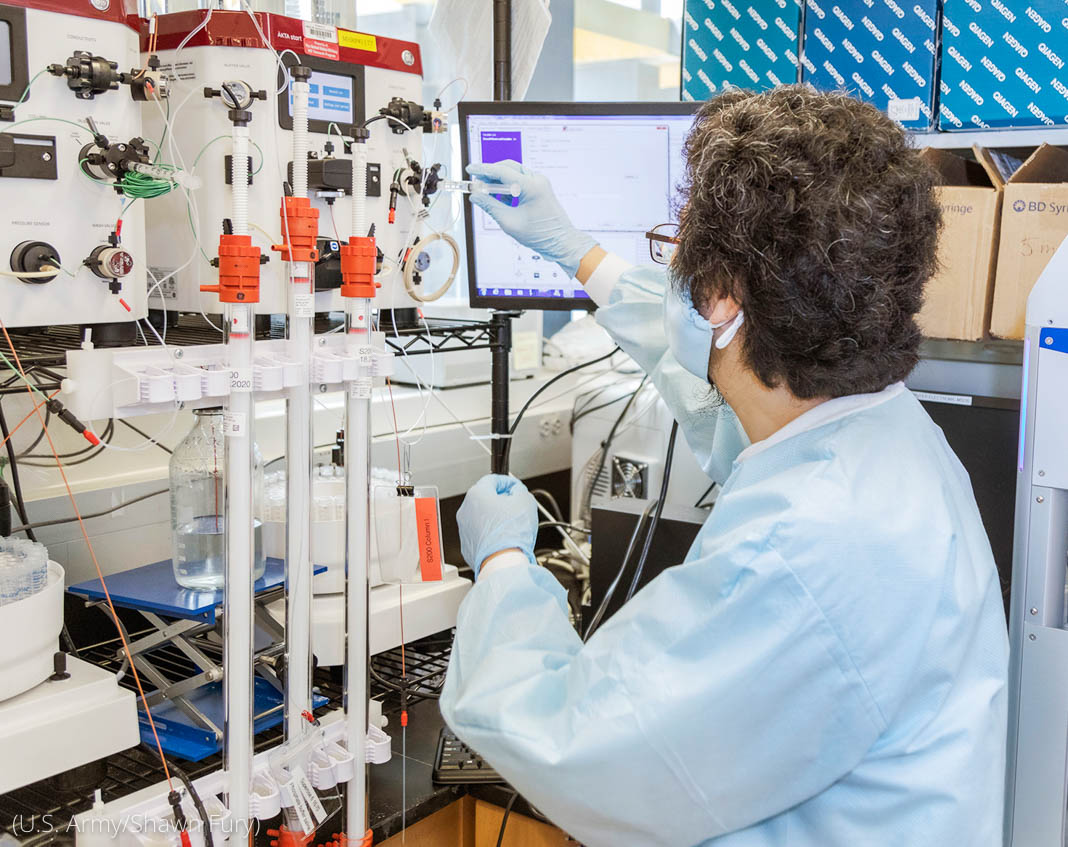
A scientist with the Emerging Infectious Diseases Branch at Walter Reed Army Institute of Research looks for a vaccine for the new coronavirus in this July 1 photo. (U.S. Army/Shawn Fury)
Modjarrad, of the Walter Reed Army Institute of Research, says that manufacturers typically wait for all the clinical studies and approvals from the FDA to be complete before making large doses of the vaccine. “That adds on months, if not years, to the timeline,” he says. Not so with Operation Warp Speed, which is partnering with the private sector to scale up manufacturing of multiple candidate COVID-19 vaccines.
By not waiting for the clinical studies to be completed to make the large doses of vaccine, “we will have vaccine ready for large populations the day it is approved by the FDA,” Modjarrad says. (Note: If it is not approved, the doses will not be used.)
What’s more, he says, “our expertise with coronaviruses; our experts in immunology, structural biology and virology; our manufacturing facility and clinical trials center have all come together to compress the timeline of vaccine development. Nowhere along the way have we skipped any steps in ensuring, assessing and reassessing safety processes.
“I cannot stress enough how controlled and regulated a process vaccine development is when it comes to safety,” Modjarrad continues. “That is the prime objective, safety, when it comes to the development of these vaccines.”
Banner image: Scientists and lab technicians in the Emerging Infectious Diseases Branch at the Walter Reed Army Institute of Research. The team is working to develop a vaccine for COVID-19. (U.S. Army/Shawn Fury)




COMMENTS0
LEAVE A COMMENT
TOP